Florida's coronavirus cases tripled in July and deaths nearly doubled. What comes next?
Zac Anderson Sarasota Herald-Tribune
Published 1:14 PM EDT Aug 1, 2020
July is coming to a close in Florida with three times more coronavirus cases than when the month began and nearly twice as many COVID-19 deaths, marking an alarming escalation in the state’s outbreak.
It was a month that transformed Florida into one of the worst virus hotspots on the globe, putting the state at the center of the debate over how to balance economic and public health.
Gov. Ron DeSantis has been among the least restrictive leaders of a major state or country, eschewing a mask requirement and allowing every business except bars to remain open. His approach largely has been to try to ride out the pandemic with minimal public health mandates.
“I think what we’ve seen is that the virus is in charge,” said Dr. Marissa Levine, a professor of public health and family medicine at the University of South Florida who leads the school’s Center for Leadership in Public Health Practice.
The rampaging virus put 12,147 Floridians in the hospital in July — an 82% increase. The 3,472 additional Florida residents who died last month equates to 112 a day, or four every hour, a grim tally that has led to increased pressure on DeSantis to take action. Florida set COVID-19 death records four days in a row last week.
State leaders face some big questions as the calendar flips to August. Can schools reopen safely? Can strained hospital systems keep up? Are more state and local restrictions needed?
Florida recorded 321,031 new coronavirus cases in July, compared to 158,997 during the previous four months combined.
If high levels of new infections continue through August, it could test the governor’s resolve to protect short-term business activity and get schools open. Many believe the state won’t get back to normal until the virus is under control, and that Florida isn’t doing enough to rein in new infections.
“An aggressive approach early, as we saw with a number of other countries, and getting it down to a level where you can control it and creating a new normal that everybody buys into is a much better way to go,” Levine said. “But I don’t know that we have the collective will to do this or the leadership will to do this, and that’s unfortunate.”
August 1 updates: State adds 179 COVID-19 deaths, surpasses 7,000
The last week of July has brought some good news, with new infections and the number of people currently in hospitals with COVID-19 declining statewide, possibly a sign that the outbreak is easing, or at least leveling off.
Local mask mandates and a more wary public that is taking more precautions may be starting to have an impact.
DeSantis seized on the glimmer of hope last week, saying he is encouraged by some of the data surrounding hospitalizations.
“Fortunately, we have seen throughout the state of Florida, statewide, we’ve seen a decline in visits for COVID-like illness to emergency departments,” DeSantis said during a visit to an Orlando hospital. “We’ve seen a stabilization or decline in the COVID hospital census at hospitals throughout the state, which again is another positive signal compared to where we were a couple weeks ago.”
But the number of new infections is still high, and it’s not clear if the downward trend will continue or if it’s just a blip. And new virus cases would have to drop substantially to truly contain Florida’s outbreak. Without a dramatic reduction, the state will see continued flare-ups that could be disruptive for the economy and health care system, Levine said.
The situation is a daunting one for health care workers on the front lines who say they are working in highly stressful and sometimes unsafe conditions.
In other news: With Isaias set to scrape Florida, Gov. DeSantis says state is ready
Hospitals strained
North Port resident June Phillips has been a registered nurse for 28 years. She currently works at Fawcett Memorial Hospital in Charlotte County.
Each of Fawcett’s 19 intensive care unit beds were occupied for most of last week, according to data kept by the Florida Agency for Health Care Administration. There was one ICU bed available Saturday.
Phillips said the hospital has been losing nurses because of concerns about contracting the virus, and because they are being overworked. Many of her colleagues have tested positive, she said.
Data provided by Phillips’ union, which gets information from the hospital as part of the union contract, shows that Fawcett currently has 39 fewer registered nurses than in the fourth quarter of 2019.
Fewer nurses means they are seeing more patients, Phillips said.
“We’ve been overworked; that’s what they do,” she said, referring to hospital administrators. “We told them time and time and time again, that, look, it is not feasible, it is not possible for us to have so many patients, six patients for one nurse; this is not a nursing home where people lay down and they don’t move.”
Asked about the staffing concerns raised by Phillips, Fawcett Communications Director Alexandria Benjamin said “The safety of our caregivers and our patients continues to be top priority at Fawcett Memorial Hospital.”
“We are actively working with local, state, and national resources to recruit additional staff to provide relief for our caregivers,” Benjamin added.
The ICU beds across all Florida hospitals were 82% full on Saturday, but eight counties, including two of Florida’s largest — Broward and Hillsborough — were at 90% or greater capacity.
Dozens of individual hospitals are at capacity with their ICUs.
There are signs that the strain on hospitals may be starting to ease. Across Florida the number of COVID-19 patients in the hospital dropped by 961 between Tuesday and Saturday, an 11% reduction.
Sarasota Memorial Hospital was down 102 COVID-19 patients Friday from a peak of 130 on July 22, and hospital CEO David Verinder noted in a video released Friday that the percentage of positive tests at the hospital has gone down.
“We’re hoping that that results in less hospitalizations coming in the next few week, we’ll have to wait and see,” Verinder said. “We’re hopeful that that’s going to be the case but we’re going to be prepared for the worst if it turns out not to be.”
With hospitalizations and new infections still high, public health experts are hesitant to confirm a clear downward trend without more data.
Worn down from treating so many virus patients, health care workers have been calling for tougher measures to control the outbreak. Last week the union representing more than 5,000 doctors, nurses and other employees at Jackson Health in Miami called on DeSantis to issue a statewide mask mandate.
“I think the statewide mask mandate would be a good thing,” said Candice Cordero, a nurse at Blake Medical Center in Bradenton, adding: “It’s frustrating for health care workers because we’re working so hard on the hospital but then we see people here in groups on vacation and they’re all out in groups with no masks and it’s frustrating to see that because people don’t understand.”
Cordero has more experience than most with the virus because of her job as a nurse, and because she was infected herself. She tested positive on July 9 and had to quarantine at home in a separate room from her family for two weeks, only leaving with an N95 mask when she needed to get something from the kitchen.
Cordero’s symptoms were mild, but it still was a frightening experience. She worried about her husband and two children getting infected, especially her 8-year-old who has asthma. They all remained virus-free.
In addition to Cordero, four other staff members in her unit tested positive for the virus during a three-week period, she said. Infections among health care workers are contributing to staffing problems at hospitals, although facilities also are struggling to staff back up after shedding employees during the state’s ban on elective procedures.
State officials have sent nurses to serve as reinforcements at Blake and other facilities around Florida. Verinder said Sarasota Memorial is bringing in contract workers “to help relieve some of our employees.”
Blake has 72 fewer nurses than in the fourth quarter of 2019, according to the union data.
“I think morale is pretty low in general because we’ve been working short staffed for quite awhile,” said Cordero, who added that she also would like better personal protective equipment, such as an N95 mask. These masks are not being provided to nurses at Blake who don’t treat COVID-19 patients, she said, even though patients in non-COVID units have tested positive.
A representative for Blake did not respond to a request for comment on Cordero’s concerns.
Levine said concerns about overwhelming the health care system should be top of mind as state and local officials plan for the upcoming school year.
In case you missed it: Trump meets with Florida sheriffs who had attended conference with COVID-positive colleague
Schools next
Cordero described her hospital as “limping along” and that seems to be an apt description for much of Florida’s health care system, which hasn’t reached a breaking point in most areas but has seen plenty of warning signs.
Levine worries that opening schools while the virus is still so prevalent could be like throwing gas on a fire, causing the outbreak to flare-up and pushing the health care system over the edge.
“The bottom line is they’ve been incredibly busy for a relatively long period of time and you don’t want to do anything that’s going to push them over,” Levine said of Florida hospitals. “and that’s got to be one of the considerations if you’re considering opening up schools.”
DeSantis said again this week that parents should have the option of sending their children back to the classroom.
“I do think there’s a lot of parents who really do need their kid to have face-to-face interactions and I think we ought to do all that we can to provide that,” DeSantis said.
Many school districts had planned to start the school year in early August but have pushed the start date back to later in the month, something DeSantis said he supports. He noted the state “may be at a much different place” by that point, saying “I think we’re going to continue to see some positive trends, at least that’s my hope.”
DeSantis added that distance learning does not work well for many children and policymakers need to be “honest about the costs involved in that.”
But there are big concerns about reopening schools, including among many teachers and parents.
The Florida Department of Education — which is run by a DeSantis appointee — ordered public schools to “open brick and mortar schools at least five days per week for all students.”
Florida’s largest teachers union, the Florida Education Association, filed a lawsuit to try to nullify the reopening order. The FEA also sent DeSantis a petition last week signed by nearly 32,000 people asking to recall the order “until the community spread is reduced.”
“Districts must have the option to protect the school year by using the less than perfect distance learning option until it is safe to return to school campuses,” the petition reads.
The DeSantis administration appears to be backing away from trying to force schools to reopen. An attorney for the Department of Education sent a letter to the Orange County School District this week saying local officials can decide when to reopen school buildings, according to the Orlando Sentinel.
But DeSantis is still pushing for classroom instruction. He held a roundtable discussion at a Clearwater school last week that focused on how schools can reopen safely.
Levine worries that opening schools with the virus still raging “could be really tragic.”
“We really need to get the cases down through the efforts that I think everybody knows needs to happen, and I hope we do that before we widely open up the schools,” Levine said.
More: Hospitals need recovered COVID-19 patients to donate plasma
Controlling the virus
Many Florida communities have adopted mask mandates and are now waiting to see how effective they are at controlling the virus. Miami-Dade County has gone further and prohibited indoor dining at restaurants.
Levine believes Florida will continue to struggle with the current patchwork approach to public health measures.
“How do you control a pandemic when you don’t have everybody operating on the same playbook?” Levine asked. “That’s why we have what we have now. If we can be more unified in our actions we can really impact this to the level we need to.”
DeSantis continues to resist new statewide mandates, though. He is touting other measures of success, such as an increase in testing.
Florida was averaging 56,485 tests a day during the last week of June. The state is now up to 81,771 on average over the last seven days of July.
But the massive number of tests has overwhelmed labs in many areas, resulting in slow turnaround times that make the tests less useful for public health purposes. Quick test results are needed to identify infected individuals before they spread the disease to others.
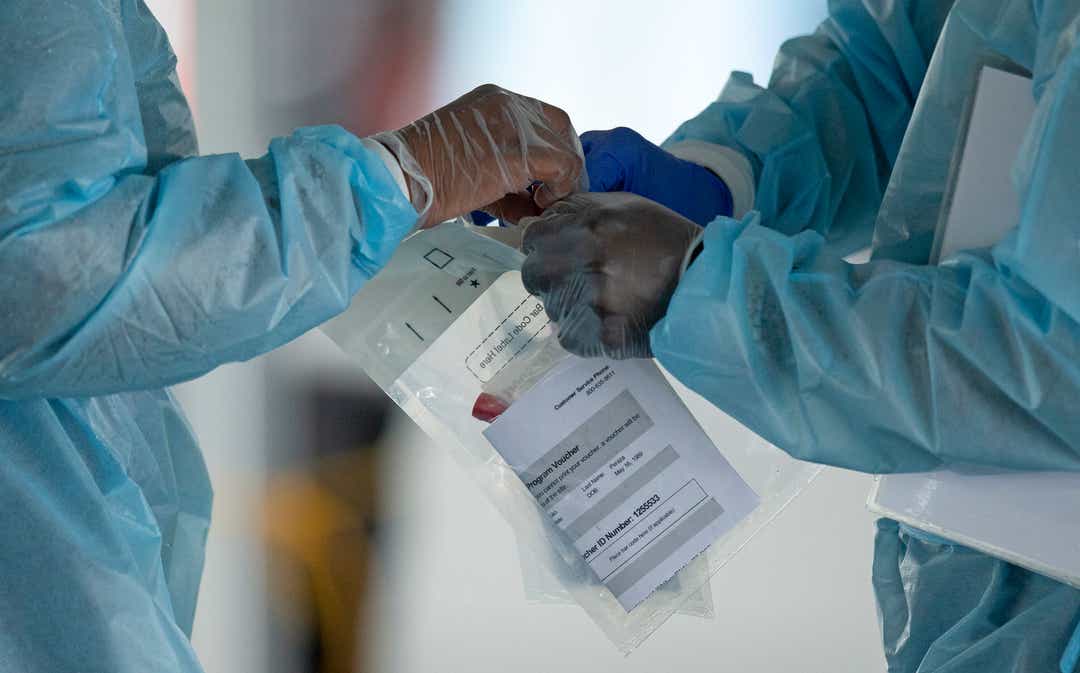
Public health officials have spent months advocating for a robust testing system coupled with large teams of workers to trace the contacts of those who test positive and get them isolated so they don’t spread the virus.
There are signs that labs are starting to catch up. Health officials in Sarasota County said test results now come back within 48 hours on average. But Levine said Florida’s entire testing system needs to work better.
“I don’t think there’s any question given the current testing capability and the contact tracing capability if the demand was lower because we had less disease in our community then those systems would work much better,” Levine said. “The challenge right now is those systems are really stressed and they’re not working.”
tinyurlis.gdv.gdv.htclck.ruulvis.netshrtco.de
